Celebrating 30 years as the nation’s most experienced developer of spine & orthopedic centers of excellence.
- 817-481-2450
- Contact Us
-
Quality Management
Quality Systems
 Large employers and managed care providers
find it amusing that while each physician group claims to have
high quality, few actually collect data or develop "systems" that
reduce treatment variation and ensure that the correct thing
is done at the right time, every time. Prizm helps physicians
and hospitals walk the talk. Prizm accomplishes this through
implementing written clinical protocols that emphasize a conservative
approach toward the use of diagnostics and surgery, which often
are over-prescribed in certain specialties.
Large employers and managed care providers
find it amusing that while each physician group claims to have
high quality, few actually collect data or develop "systems" that
reduce treatment variation and ensure that the correct thing
is done at the right time, every time. Prizm helps physicians
and hospitals walk the talk. Prizm accomplishes this through
implementing written clinical protocols that emphasize a conservative
approach toward the use of diagnostics and surgery, which often
are over-prescribed in certain specialties.
Prizm also helps the provider measure clinical outcome and collect valuable case management data that aligns the organization to the employer referral source.
Spine Care Quality Defined
Quality is defined as the reduction of variation around the mean. More specifically, in the field of spine care, there are a lot of people measuring the WRONG things, or looking at the telescope through the wrong end.
Fact: Most of the existing spine outcomes systems are not measuring what consumers, employers & payors want to know. For example, most of spine outcomes focus on hospital-side outcomes. However, 90% of spine care is NOT SURGICAL.
The educated payors do not desire a ranking of surgical mills that operate unnecessarily on patients. We know that as a “outcomes fact.” Over 20 years, Prizm has conducted more than 500 one-on-one meetings with health plan medical directors, health insurance VPs, benefits VPs at large Fortune 500 companies and case managers for work comp companies.
Outcomes fact #1
Many payors actually view the spine surgery patient as a “failure” because outcomes from fusions are poor, and spine surgery can be expensive with way too many patients progressing only to pain centers and other invasive procedures related to “failed back surgery syndrome.” According to Dartmouth Medical Atlas, which is used by payors and government payors as the definitive source for information about treatment variation, spine surgery in the U.S. is highly variable and done excessively, compared to other countries. Consequently, payors — and now consumers — all want to know who is best for treating back & neck pain — without surgery. Consumers in particular are educated to search for experts in NON-surgical spine care.
Outcomes fact #2
90% of back & neck pain can resolve WITHOUT surgery. Yet most of the current outcomes systems don’t track the percent of patients that receive and then recover with non-surgical treatment options like spine therapy or injections.
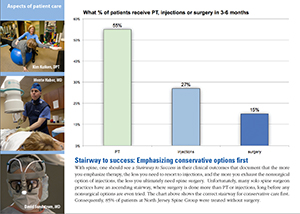 Case in point: The attached chart from Prizm’s outcome system shows the correct DESCENDING STAIRWAY TO SUCCESS that should be evident in a spine center’s outcomes tracking. This stairway documents that the more you use NON-surgical treatment options like therapy, you will achieve symptom relief for some patients and fewer will then need injection therapy. Of those patients who do receive injection therapy, some will have symptom relief and never need spine surgery. This stairway documents the benefits of the Prizm spine center model based on the three-legged stool composed of spine therapy, PMR for injections, and lastly spine-specialized surgeons.
Case in point: The attached chart from Prizm’s outcome system shows the correct DESCENDING STAIRWAY TO SUCCESS that should be evident in a spine center’s outcomes tracking. This stairway documents that the more you use NON-surgical treatment options like therapy, you will achieve symptom relief for some patients and fewer will then need injection therapy. Of those patients who do receive injection therapy, some will have symptom relief and never need spine surgery. This stairway documents the benefits of the Prizm spine center model based on the three-legged stool composed of spine therapy, PMR for injections, and lastly spine-specialized surgeons.
Outcomes fact #3
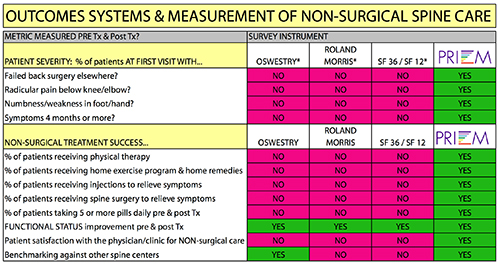
Few outcomes systems track patient severity at intake, or the percent of patients dependent on pills pre & post treatment.
The attached diagram shows that Prizm’s outcomes system which has been in use for 15 years, is the only one in use today that tracks all the desired metrics. True, the Oswestry has more than 30 years of historical data. But we would argue that this data represents 30 years of tracking things that aren’t relevant to the future of spine care. At what point does a forward-thinking provider of spine care unhook from systems that don’t track what the customer (patient) and payor (insurance company/employer/government) want to know to determine value and quality in the future. The Oswestry produces an arcane functional score BEFORE treatment, and then another score after treatment. Aside from the sampling bias that also occurs with this system based on if the center is truly doing outbound interviews on a random sample, or auditing a biased group of people that happen to respond to mail or surveys, the scores don’t reveal use of pills, return to work, residual neurological symptoms like ongoing radicular pain or numbness in a foot or hand. And worst of all, the Oswestry doesn’t track what percent of patients ultimately receive surgery at a center.
Outcomes fact #4
Besides surgery, we know that the other thing killing payors is pharmacy costs for spine. Consequently Prizm measures both surgery rate and use of pills, pre and post treatment.
Outcomes fact #5
Most outcomes systems have “sampling bias” because they limit their audit to only those patients who return to that doctor’s office for follow up. That’s bias. Prizm systems avoid this bias by having an RN who calls a random sample at home.
Prizm’s outcome systems do not try to be all things to all people. We recognize that the surgical encounter is equally important and there are systems that do a better job at that measurement. We applaud them. With that said, and with 20 years of spine experience and data from the best multi-disciplinary spine centers, we know for certain, the ideal surgical rate for a TRUE respected spine center is between 8 and 13 percent of patients. Yet most surgically oriented practices can be almost triple that — and with a LESS COMPLEX patient severity than these mature spine centers that attract patients from 200 miles out. And that sadly, is outcomes fact #6.
Right now, the spine market is in transition. Payors are now myopically shopping for spine surgery on a discounted case rate. But soon they will learn that not all these patients even needed surgery in the first place. Some would actually become asymptomatic through a true multi-disciplinary spine center with PMR and spine therapy. So the first phase of evolution is now shopping the surgical mills. The end phase is steerage to disease management centers of excellence that resolve some patients non-surgically as well as with surgery. That is the ultimately the best value. And that is what a strategic plan for spine should address, rather than building an out-of-date Edsel.
Our conclusion and prognostication is that all the existing spine outcomes systems will likely be replaced by a national system — like the JD Powers study of automotive quality — that audits from the outside the efficacy of both non-surgical and surgical care. In the meantime, pressure will be on spine practices to demonstrate they understand, and can provide, NON-surgical treatment options for the 90% of back pain sufferers, rather than documenting and showcasing a bias toward surgery.
Why it’s important
 Detecting quality is important because with the tremendous advances
taking place within the medical field today, healthcare consumers must
know how to benefit from them. You must take an active role. The best
healthcare will not find you; you have to seek it out.
Detecting quality is important because with the tremendous advances
taking place within the medical field today, healthcare consumers must
know how to benefit from them. You must take an active role. The best
healthcare will not find you; you have to seek it out.
Not only is quality healthcare of obvious value to individual consumers, its permeation into the market will continue to benefit society as a whole. As more and more people begin integrating prevention methods to avoid health problems, unnecessary medical costs will be saved.
While the United States offers the highest standard of healthcare in the world, there is still huge treatment variation based on the doctor you see. The truth is that your choice of physician will determine the quality of care you will receive.
A center of excellence approach
Centers of excellence allow physicians who are super-specialists within a given medical niche to come together and merge their abilities, automatically resulting in a high quality provider.
Physicians and therapists work together with a team approach. Their collaboration creates personalized treatment plans that reduce time away from work. Our specialists glean information from the results of diagnostic tests to learn key information specific to the patient, eliminating unnecessary testing and incorrect diagnoses. This evaluation allows us to modify treatment to cater to specific patients, thereby removing unneeded fees and treatments.
When trying to maintain a high level of care, everyone involved should be able to see the big picture of what they’re trying to accomplish along with how they can best serve patients and beat out the competition. In addition to direct marketing strategies that target employers and managed care, a center of excellence must position itself in its regional market as the single expert source for information on back and neck pain. By offering a comprehensive menu of specific information on their Web sites, health care practices educate patients, ultimately helping reach the primary goal of providing the best, most accurate care.
Reduce treatment variation with clinical protocols
 Many specialties have
wide treatment variation and sub optimal care. The first step
to improving care through a center of excellence model is to
work with the physicians involved to develop uniform clinical
protocols that reduce treatment variation. Then by collecting
data and comparing clinical outcome and functional status, treatment
can be improved.
Many specialties have
wide treatment variation and sub optimal care. The first step
to improving care through a center of excellence model is to
work with the physicians involved to develop uniform clinical
protocols that reduce treatment variation. Then by collecting
data and comparing clinical outcome and functional status, treatment
can be improved.
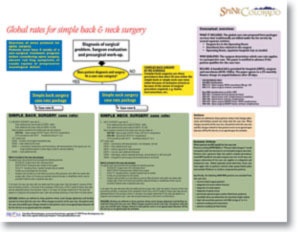
Prizm has developed proprietary binary path protocols that enable physicians to unify their care and ensure that individuals are getting the right thing at the right time every time, which is the end goal of any quality improvement endeavor. Further, Prizm's protocols enable a center to take a pre-set price for an episode of care.
Disclaimer:
The pictures displayed in this website are images of physicians, patients and employees who have consented to have their pictures in this website.
HAVE A QUESTION?

Wouldn’t it be convenient if someone created a listing of spine centers of excellence across the United States that all emphasize non-surgical treatment options before surgery?
Finally, there is a place.

Centers for Artificial Disc is the only verified national listing of spine centers that specialize in artificial disc replacement surgery.
CentersForArtificialDisc.com